Addiction affects your brain and body too, which is why detox is just the first stage of recovery

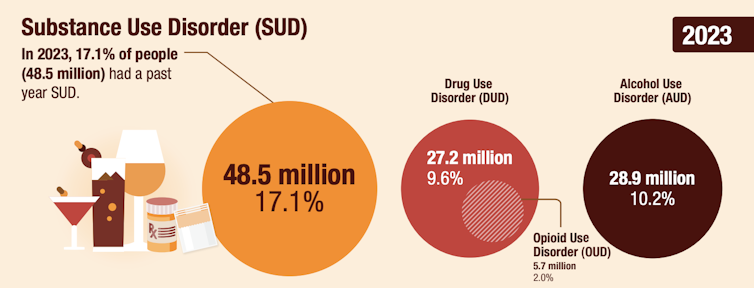
Addiction is one of the most common and consequential chronic medical conditions in the United States. Nationwide, more than 46 million people She met criteria for substance use disorder As of 2021, latest data available.
Decades of evidence show that addiction is a chronic, relapsing disease Brain disease. However, there is still a broad audience Misunderstanding of what constitutes “treatment” for addictionNot to mention Heavy stain associated with it.
Many patients, families, and even healthcare systems view admission to a detoxification or medically managed withdrawal unit as an essential step in recovery. Sometimes, this first step is all that is needed. your Physician and fellow in addiction medicineI know firsthand that this common perception is wrong, and that it perpetuates misinformation about evidence-based treatment.
Centers that provide medically managed withdrawal are designed to stabilize patients in crisis, safely manage acute withdrawal and stop dangerous patterns of use. However, the idea of “detoxing” Equivalent to recovery It has taken over over the past few years. This belief appears to be rooted in outdated models of addiction, general misunderstanding, and addiction Media photography It frames addiction as simply a problem of physical dependence.
Detox is the starting point, not a treatment plan
It is not uncommon for patients to present to medically managed withdrawal, more commonly known as “detox,” without a post-discharge plan. “I didn’t think that much,” or “I just want to get over this,” or “I’m in treatment now, right?” are some of the responses I hear often.
However, this first step is only the beginning of recovery. Detoxification from alcohol or Benzodiazepines – These could be medications known as “benzos,” such as Xanax, Ativan, or Valium Dangerous or even fatal If not administered in a medical setting. While detox is often necessary to get someone out of withdrawal safely, it only treats the short-term physical symptoms, not the underlying addiction — nor does it address the factors that lead people to problematic alcohol and drug use.
His addiction The causes are neurologicalPsychological and structural. Addressing these drivers is as important as managing the initial withdrawal. Medically managed withdrawal does not restore neurochemical imbalances, provide long-term relapse prevention strategies, or help patients manage ongoing life stressors or triggers as they arise.
In a 2023 study of adults with opioid use disorder, relapse rates after six months of treatment were highest among individuals. Who received only short-term inpatient treatment77% of these patients returned to using it. Relapse rates were significantly lower among those who remained in inpatient care longer or who transitioned to outpatient treatment after short-term inpatient treatment.
When people were also treated with a long-acting type of opioid blocking medication called naltrexone, relapse rates dropped across all settings — to 59% after short-term inpatient care, 46% after long-term inpatient care, and 38% among those treated as outpatients. These findings highlight that brief detoxification without ongoing care is often insufficient to support lasting recovery.
However, many centers that provide medically managed withdrawal face clinical, regulatory, and financial constraints. As a result, they often have limited resources and can only accept patients for three to five days. In these circumstances, centers work primarily to stabilize acute withdrawal symptoms rather than focus on the underlying factors that may prompt drug use and potential relapse.
US Substance Abuse and Mental Health Services Administration
Why does addiction not end after withdrawal?
Addiction is a chronic and sometimes relapsing condition. He – she It disrupts three interconnected systems in the brain:
– Bonus track, which Dopamine, a neurotransmitterIt works on the pleasure centers in the brain.
– Centers of tension in AmygdalaIt is the part of the brain that processes emotions such as fear, aggression, and anxiety. and
-Stimulation and control systems Prefrontal cortexwhich manages high-level executive functions such as planning and problem solving.
When individuals repeatedly use substances such as alcohol or drugs, they may discover that things they once found rewarding or pleasurable can no longer compete on the same scale. This often leads to increased stress and poor self-control. Their bodies reduce the number Dopamine receptors – Sites in the brain that bind dopamine – As a result, previously motivating and joyful activities seem depressing.
This is what happened to a patient who told me: “After using methamphetamine, everything became chaotic and nothing made me happy.” Initially, methamphetamine use creates a state of “high” or euphoria. Over time, people use it simply to avoid getting sick. The once cheerful material becomes the proverbial ball and chain.
These neurobiological changes don’t happen overnight, and neither does recovery. It is unrealistic to expect that a typical admission of medically managed withdrawal, which may last only three to five days, will lead to healing of patients’ damaged circuits.
Furthermore, some symptoms can persist, such as anxiety, mood changes, difficulty sleeping, and general dissatisfaction with life Three to six months or more After the initial withdrawal period. Cravings, which are intense psychological urges, often arise without warning. When this happens, having recovery support systems, such as a sponsor, mental health professional, or relapse prevention plan, can be crucial.
Addiction is often rooted in aggravating factors such as anxiety, depression, trauma, chronic stress, and pain. For example, chronic pain resulting from a previous injury can often lead to misuse of prescription opioids, which you may later develop into using Other substances such as heroin or fentanyl.
Patients with substance use disorders often rely on substances as a way to escape from these deeper problems, rather than developing healthy coping mechanisms. All they knew in times of suffering was their medicine of choice.
Often It requires months or years To develop new ways of thinking, emotional regulation, habits, and responses to trauma after leaving a history of substance abuse behind. Learning to live without substances and without change can be a new and terrifying concept.
Post-detox treatment
If medically managed withdrawal is just the first step, what should come next? Patients may consult with their doctors and choose to begin medication-assisted treatment, which helps prevent cravings and withdrawal while addressing deeper issues through mental health treatments such as: Cognitive behavioral therapy. Opioid use disorder It is treated with medications such as buprenorphine or methadone Alcohol use disorder Medications include naltrexone, acamprosate, or disulfiram.
These medications are at least as effective as many standard treatments in medicine, and I believe they should be considered where appropriate. There are medications to treat alcohol use disorder Proven effective In reducing the risk of death and hospitalization, but this Medicines are often underused.
Treating substance use disorders is similar to managing diabetes, high blood pressure, or other chronic health conditions. Even after patients emerge from the impending crisis, the work continues.



